I've been so humbled and honored that others have messaged me for advice on their health journey. I have to admit I've been a little overwhelmed wanting to get back to each person and tell them everything that was helpful for me while also trying to make sure I'm still resting and recovering from my surgery 6 weeks ago. I just remember how valuable time is when you are suffering and so I didn't want to make anyone wait for a response when they are trying to figure out what to do. The wait time for doctors and tests take so much time in itself.
I decided it might be easier if I wrote everything that I wished other warriors would know as they begin their fight or deciding on surgery. I also had a few older posts that I felt could be useful for my new readers that just came across my blog so I will link them in here too. Additionally I have been working on a few posts documenting more specific details about my diagnosis and treatment in Germany.
- My first question. Do you know if you have EDS or know what that is? If not, are you hypermobile or very flexible? I ask this because there seems to be a connection between Ehlers-Danlos Syndrome and multiple vascular compressions. Here is a post if you are curious about getting diagnosed and this is a more detailed post after I finally got diagnosed.
- If you do believe you may have EDS, a valuable resource who I'm very excited has come out of retirement to help others again is my geneticist, Dr. Golder Wilson. For $100 (although not covered by insurance I think his services are worth way more than this), he will send you a detailed packet for you to fill out and return to him where he will write up a report for your doctors. He used to do this along with genetic testing, but he found that most doctors didn't believe or trust the findings so he didn't feel like his patients should waste money on something if it didn't help their health problems be taken seriously. I want to also add that he has EDS himself and his evaluation was a huge tool for me to understand what can be connected and caused by EDS, but also give you some direction on how to deal with these issues. Here's his website: https://www.kinderggnome.biz/index.html
- If you do want to get genetic testing for peace of mind and to finally have proof of your diagnosis, he does mention on his website that you can look into Invitae, which does a blood test to rule out any other forms of EDS besides the hypermobile type (what I have that doesn't have a genetic marker discovered yet). The Invitae test is actually what my rheumatologist did for me and is at least not outrageous even if your insurance doesn't cover ($250 through doctor and $475 for self pay).
- Why I believe you should know if you have EDS before looking more into vascular compressions is that it'll clue you in that you are more likely to have multiple compressions and help you understand what is causing them. It also will give evidence to some of the other unexplained problems you may have or give you a heads up what you could be at more risk for. A couple of these are that we over metabolize or don't metabolize certain medicines, anesthesia/epidurals may not even work, we can form keloid scarring, and we can be very slow healers.
- Next, I think it's important to join the vascular compression groups on Facebook. It's wonderful the community we find and support just meeting others that have gone through something similar and relate to each other's journey. They also have so much information to give you a direction or warnings on what doctors to seek out or what testing and surgery to get. There are usually multiple groups for each compression out there.
- The biggest thing I want others to know when they reach out to me is that no matter what you decide, even if it's different doctor or treatment than I chose, I will always support you. These decisions are so very tough and what is right for one person, may not be the best option for someone else because of location, finances, previous surgeries or just goals for treatment. What makes it so difficult for us that experience these rare illness is that we don't necessarily know how long term the surgery results work for with any of the treatments out there right now, but we unfortunately are not in a place where we can't not do something and risk further damage to our health.
- What I have found the best thing that we can do is to find a surgeon who you trust and really cares, but that also is willing to continue learning and adapting. Sometimes complications happen at no fault of the patient or surgeon's, but sadly not all doctors are willing to admit a problem or willing to help you afterwards. This is why other's experiences can be helpful. Just make sure they are coming from someone who has had an actual experience with the surgeon and not just hearsay.
(source)
- Something also critical I've learned along this journey is that you need to ask a medical professional those hard questions. Asking them to explain about the compression, or why they do a surgery, why that specific surgery, or what their success rate is. I used to be so afraid because I didn't want to come across that I thought I knew more than the doctor or step on any toes and offend him or her by making them uncomfortable. I finally realized that if they don't react well to those questions than that is a huge red flag and they are not the right doctor for me. I'll never forget what my counselor told me after I had a very negative experience with one that I wrote about here. He told me the doctors work for me and I can fire them. It sounds so simple, but when you've been to doctors over and over again for so many years, a lot of us get so nervous anyway that it's difficult to advocate for one's self. What has changed is that I ended up realizing that there were a lot of times if I didn't appreciate the research and knowledge I had, then I would've missed out on other possibilities or help for my health. An example is when a doctor told me they didn't think I had the compression and they wouldn't do my surgery. I knew that doctor after telling me that was immediately about to get off the phone and that's when I said well then I need these referrals and these tests because there is a problem, and it needs to be fixed. After the phone call it just made me so angry and upset for the people that unfortunately believe their doctors that there's nothing else to do and there is nothing wrong.
- Depending if you've just been given a diagnosis by a doctor and never heard of this compression, you've had issues for years with no answers so started doing your own investigation and stumbled on this diagnosis, or you've been through the ringer and had multiple surgeries already but still having issues, I would first want you to be aware of all the compressions out there and their symptoms. What I want to prevent is you only knowing about just MALS or just Nutcracker so you go straight to surgery, only to then have other symptoms that become just as worse, and find out you actually had two or more compressions.
- I'm a visual person so I know it helps looking at where these things are located and to have a little key for what the most popular compressions are. If you are going, "um, you lost me" haha then start with this post where I shared a couple videos.
- My next question is do you currently have a doctor that listens to you, is willing to help you, or actually knows about these compressions? Did they immediately request for you to do a color Doppler ultrasound or CTA? (Now just because your ultrasound or CTA came back "normal" does not mean you do not have a compression, it can mean the right person hasn't looked at it to diagnose). This happened to me. Multiple times and multiple imaging came back "normal" when my surgeons told me that my Nutcracker was the worst they've seen.
- A very popular diagnostic tool or requirement before surgery in the US is a venogram. They are usually done by Interventional Radiologists. I had 3 of them and was not aware that they can damage your veins and can easily miss a compression, especially if it's not a tilted venogram. This is when I will now advise if you have been diagnosed or think you have PCS or NCS, please please please do your research on coils and the complications.
If you are still curious or would like to know what I mean, don't hesitate to message me before going down this route. NEVER agree to do your first venogram where you are put under and the doctor says if he finds something he will take care of it. Please speak up beforehand and say that no matter what is found, you want to stop the operation and be told so you can have time to think on the treatment. I hate mentioning this, but I have heard horror stories of a few women believing they were just doing a diagnostic venogram and wake up with 20 coils put in or a stent for their renal vein compression.
(source)
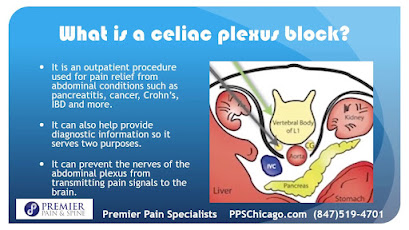
- The other diagnostic tool in the US that a lot of doctors also require is a celiac plexus block. The belief is that if you get around 3 hours of relief, that the surgery should be recommended and will also give you relief. A couple things to be aware of: a block can cause some scar tissue which means more to remove during surgery, a block can be done incorrectly so the best thing is to find a reputable pain management specialist who has done many of them, after the block unfortunately the pain is much much worse and I've been told to be prepared for pain killers or something to help with relief. If you can request that the block be done with a steroid or something to help with longer relief, this has been shown to be helpful to patients.
- I believe knowledge is power so the best thing you can do is look at journals or scholarly research and studies, talk to others in the compression groups, ask your own questions in a post, or specifically search for a certain popular doctor, certain surgery type, or someone you know that's had a certain surgery or doctor to see their journey. You can search my name as well to see where I reached out to the community to get a lot of feedback and direction.
- You are not alone. You are not crazy. There is hope.
- Sometimes it's hard for me to want to speak about how well I'm doing and my surgery success because I know how difficult it was for me to hear others who seemed to have it much easier. I was of course so happy for them to find a doctor to help them or get surgery to fix their pain and symptoms, but when I would have so many closed doors I couldn't help wonder why and at times I couldn't take their positive news because I just wasn't sure if it would ever happen for me. If you are feeling like that, it's ok. There are so many emotions with these illnesses because sometimes it makes us feel so crazy. Symptoms not being constant can mess with your mind. Doctors not believing how bad your pain is or how debilitating the symptoms are can mess with your mind.
(source)
- Something wrong that happens quite often with these compressions is that they often get misdiagnosed with depression, anxiety, or an eating disorder. I will tell you that I had doctors think my pain was caused because I was depressed so I finally decided to start going to a counselor so that they would stop trying to get me to take medicine for that. Yes, those are very real disorders and issues, but because the doctor doesn't understand what a compression entails, they try to give you an "easy fix" or pawn you off because they don't know what's wrong, is unacceptable.
My counselor actually became one of my biggest supporters on my journey so I hope by being vocal about my experience that it helps with the stigma. He gave me some of the best advice as I sought answers. Please also know that it is quite understandable to have depression or anxiety when dealing with chronic pain. How can it not get to you, especially when others don't believe your pain or doctors won't help you. I see you. I believe you.
- I kinda shook my head after my surgery when I realized how many of my symptoms were gone. Ok like all my symptoms were gone. It just showed me how many things are affected by lack of blood flow. It's shocking, and so many doctors just have no idea. My surgeon did though, and I'm so very thankful for his understanding of his patients and their pain.
(source)
- Now if you get to a point where you can't find a doctor who believes you or wants to help you, I recommend you get a CTA done requesting a certain protocol that's actually the opposite of a normal CT where it's done on exhale. It doesn't have to be ordered by a vascular surgeon or anything, if you can get your GP or someone, that's perfect. Make sure you get multiple copies of that CD.
- Side note: Start getting print offs of all your reports, tests, anything from your doctors (I know sometimes you do have to pay, but it's worth it). Keep it and any imaging CD's in a binder. First off it'll be something you have for any ER visits and second, bring that bad boy to every appointment, especially if it's a new doctor. The more complicated you get with more diagnoses or adding multiple specialists to your team, the bigger your paperwork trail will become and so many times I've saved myself at an appointment when a doctor asks about a past diagnosis or test and I can bust it out of my binder on the spot because usually even when I request doctors to fax or send records to a new doctor, the office does not do it and I would've had to make another appointment for when they finally had the documents or information. So that's a little tip I'd recommend, but I have feeling most of you have done this already without being told :)
(source)
- If you can't get a diagnosis or help with treatment, but get your hands on your CTA, I would recommend an online consult with Professor Thomas Scholbach. A trip to Germany where he can do his own ultrasound would be best case scenario, but when I did the consult first, he saw things on my CTA that no other doctors had. You can send additional imaging for an extra fee and here's his website if you are interested: https://scholbach.de/ If you would like to know more about him and Professor Sandmann, you can also read my Germany FAQ post.
- The reason I recommend this is I want to make sure you don't have a compression missed. Also, his very thorough report (with pictures, measurements, and diagnoses sent to you beforehand) may help you have doctors reevaluate helping you or accepting you as a patient for their surgery. He was also the first doctor that I came across who wanted to understand why these compressions were happening and look at the body as a whole, not just each compression. When I asked him a question he could give me multiple answers backed up with different publications or research from different countries and languages.
- Another thing I did on my own was buy reagent strips that you can get anywhere. They are the same strips doctor's office uses to test for protein or hematuria. A lot of us with Nutcracker actually have traces of blood in our urine so when pain is severe, I would recommend doing this on your own if it hasn't been shown in other previous tests and you can tell it looks darker or has a funny smell at certain times. It's another symptom that can help get your diagnosis. [As an Amazon Associate I earn from qualifying purchases #paidlink]
- Ok this is the time I want to really get into the compressions. Back in February I wrote this post to break down what they are and what my surgery options were. Depending on what compressions you do have and how many, it usually comes down to deciding if you want to do one surgery to fix all the compressions at once or multiple surgeries to fix each compression at a time and see if the other compressions happen to resolve on their own. I contemplated all scenarios. My first choice doctor I hoped could fix all my issues in one surgery, ended up retiring while I was on his wait list.
Next, I sought out MALS specialists in hope that fixing the highest compression might take care of my lower compressions without further treatment. Unfortunately I could not get a MALS specialist to help me or agree to do a block and that's when my plan was to find an AT specialist and even started thinking about nephrectomy because it seemed like all the experienced surgeons weren't taking new patients (I found out we are usually told that we aren't candidates for donating a kidney). More dead ends. That is when I finally did an online consult with Scholbach because I had started vomiting the last couple months along with having kidney stones so we knew I couldn't keep waiting around.
- If you are like me and have noticed some medicines don't help at all, or you have very strange reactions, then I would suggest getting a genetic blood test done to show this as proof. This is a good idea before you have surgery, that way you know what works the best to put you out and for pain relief during recovery. I had begged multiple doctors to do this test because I had a lot of eye rolls when I would explain not being able to take certain medicines, but then my EDS doctor did it first appointment without even asking her. Sure enough, the report lit up like a Christmas tree. Here's the one that I had done: https://blog.genomind.com/medication-metabolism
- Another syndrome that usually goes hand in hand with EDS and can actually be caused by vascular compressions or pelvic congestion is called Postural Orthostatic Tachycardia Syndrome (POTS). Do you feel dizzy or lightheaded when you stand (or even have a history of passing out)? I've been planning to share about it next month for Dysautonomia Awareness Month, but I had a friend who thought it would be another important thing to bring up in this post because so many of us have to use a cane or wheelchair prior to surgery. I agree, I don't know any of my friends with vascular compressions who did not have orthostatic intolerance. You can get a tilt table test done to get diagnosed, which is usually done by a cardiologist.
- If you believe you have SMAS, and insurance is not covering doctor appointments or you need assistance because you are having to travel to a specialist, please look into filling out a grant from the SMAS Organization. If you'd like to donate to a great cause, this is one! They sell different things to help raise money for the grants and the charity we use for our smile.amazon.com, which donates a portion of the proceeds.
- The last thing big topic I'd like to discuss that also goes into the next tips I'll give is Physical Therapy. Even if you have never stumbled on Scholbach's website and his research about spinal issues causing the compressions, you may have discovered on your own to have back pain or told you have lordosis or scoliosis. This happens to also tie into the connection with EDS. It all supports how important correct posture, body alignment, and strength are for our bodies. My physical therapist was actually the first one who brought up the term Pelvic Congestion.
Now, I don't recommend just any PT because some can actually be more harmful if they are not educated or experienced with EDS or compressions, but the ones that are, they can not only help rule out other issues like pelvic floor/bladder dysfunction or prolapse, but they can help with pain relief (doing massage or visceral manipulation) and showing you beneficial exercises. If you'd like to locate a qualified PT, make sure they are trained in IPA (list of therapists here) and have a CFMT background.
Something very important that myself and others who've had the surgeries try to caution is the only reason you should contemplate these vascular compression surgeries is if you are severely debilitated and your quality of life is impacted. Although I am doing well, the surgery always poses risk with the areas they are fixing, and the recovery can be very difficult (although we usually feel worth it to get a chance at living life again).
While you have pain or are suffering in the meantime:
I was surprised at how many things I did on my own naturally to help with blood flow before finding out they were things that do actually make a difference and can help take the edge off.
(source)
*Most comfortable position - laying down on left side, curled up, or child's pose
*Epsom salt bath - something about being in that hot water (would be my go-to for the really bad times)
*Heating pad (I kinda feel like that could even be a diagnostic criteria, like are you attached to a heating pad whenever you are at home? - check - you have a vascular compression)
*Cane or shower chair (I was too proud for awhile to use these, but they were lifesavers)
*Compression socks (not the medical grade, with my EDS I can't use those, but these on Amazon really helped, and a ton of cute options as well) #paidlink
*Unfortunately no foods in particular were easier on preventing pain. Shakes and drinking anything were just as bad for me. I would make sure to eat high nutrient/calorie foods to keep on as much weight
to stay strong for surgery. If you need guidance on foods or supplements or even considering tube feed, my cousin is a Nutritional Therapy Practitioner and can definitely help you (plus, she knows what chronic illness is like first hand). She has a lot of great tips she shares on her Instagram for free just to help others while she's going to medical school.
*If you do have POTS, hydration is important (if you are able), but more importantly upping your salt intake and electrolytes can make a big difference in symptoms. The best that I've found and use are Salt Sticks or Nuun #paidlinks
*CBD Oil (specifically Charlotte's Web because I've tried others without the same result) has been a huge benefit for me for different reasons, but a big one is to help keep me regular with BM's on pain medicine. Even after surgery I had a BM on the 3rd day, which in the past with things like Colace was fortunate on Day 7.
*If you can get your doctor to prescribe you Cialis (Tafalidil), it's a vasodilator, and had been used at UofW even as a diagnostic tool and when I finally got a doctor to agree to try showing this study, I was amazed that it helped! I took 5 mg daily and if you are in unbearable pain, it's worth a try. Because it's off label, I couldn't get insurance to cover, but if you use a GoodRX code, I was able to get the price down to $14 for 60 pills.
*For nausea with my experience from 2 sick pregnancies, I knew the only thing that would help was Phenergan (Promethazine). Again, I have weird issues with certain medicines working so Zofran and the other 5 popular ones I went through gave me no relief.
*If you are able to, doing exercise and strength will help your body prepare for surgery, but I do know for some, exercise increases symptoms and pain. If you do not have a physical therapist and are able to workout, I recommend Jeannie Di Bon (especially if you have EDS). You can try out some of her free videos like above first before paying for one of her courses. Even with my exercise science background and personal training past, I learned things that I didn't know along with helping with pain I previously had in my shoulders.
[Medical Disclaimer: The content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. My hope is that it'll provide you direction on finding the right doctor to receive diagnosis & treatment.]
Are there any questions or specific information I left out that would be most useful to you or you think someone should know?
What has been the biggest guidance or wisdom for you on your path to diagnosis and treatment?









1 comment:
Thank you so much for taking the time during your recovery to post this. So much great info for those of us still trying to figure this out. I hope and pray you continue to heal and enjoy life 2.0!
Post a Comment